Scientists track Parkinson's journey from gut to brain in mice
27 June, 2019
The theory that Parkinson's disease can start in the gut has gained further support in a recent study in mice. Scientists prompted toxic protein to form in the gut and tracked each step of its journey to the brain via the vagus nerve.
Researchers at the Johns Hopkins University School of Medicine, in Baltimore, MD, conducted their investigation in a new mouse model of Parkinson's disease.
The new model replicates a number of early and late signs and symptoms of Parkinson's disease, including some that are not movement-related.
The team found that they could get the mice to develop these features by injecting their guts with "preformed fibrils" of alpha-synuclein, the protein that forms toxic clumps in the brains of people with Parkinson's disease.
A paper that appears in the journal Neuron describes the mouse model and the study findings.
"Since this model starts in the gut," says co-senior study author Ted M. Dawson, who is a professor of neurology at Johns Hopkins University School of Medicine, "one can use it [to] study the full spectrum and time course of the pathogenesis of Parkinson's disease."
He explains that such a model could allow researchers to test ways to halt Parkinson's at different stages, from before symptoms emerge to full-blown disease.
Parkinson's, the gut, and alpha-synuclein
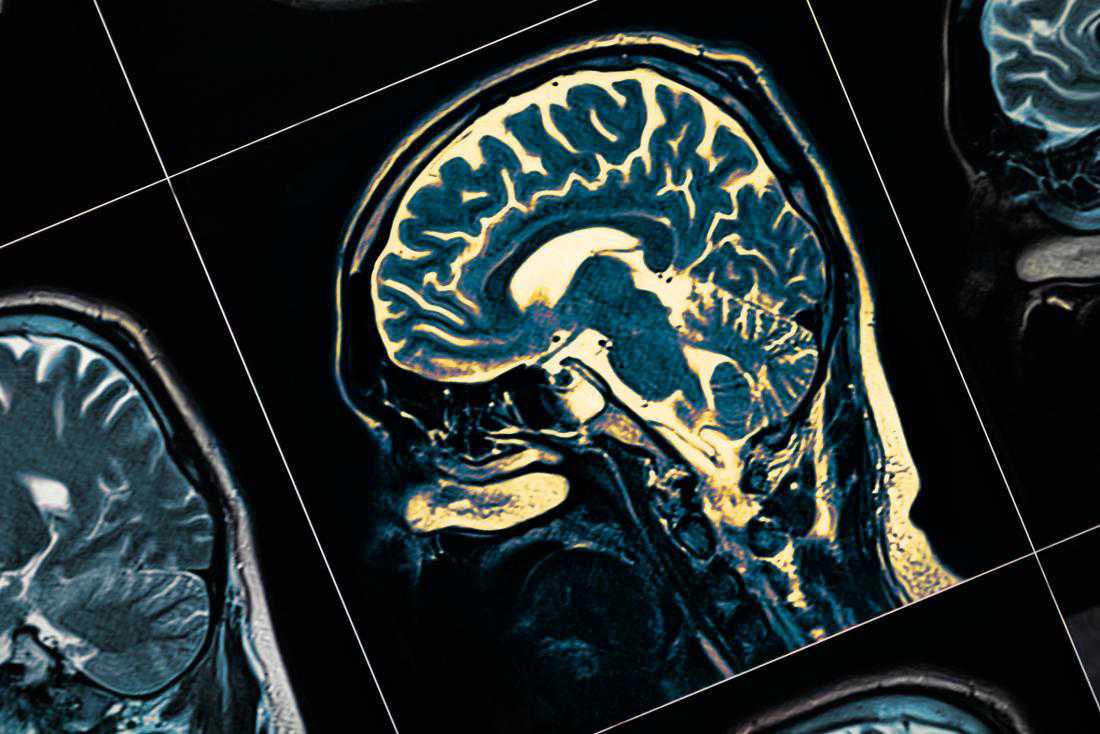
Parkinson's is a disease that progressively destroys brain tissue. It kills brain cells that make a chemical messenger called dopamine that helps with motor function, or movement control.
A hallmark of Parkinson's disease is the clumping of badly-folded versions of alpha-synuclein protein in the affected regions of the brain. Pathologists have observed these clumps in post-mortem brain exams of people with Parkinson's disease.
The main motor symptoms of Parkinson's disease include movement that is slow, stiffness, rigidity, tremor, and balance problems. Difficulties with swallowing and speaking can also occur.
Symptoms unrelated to motor function can also arise in Parkinson's disease. These nonmotor symptoms include pain, fatigue, mood disorders, excessive sweating, losing the sense of smell, problems with planning and attention, constipation, and sleep disturbances.
As yet, there is no cure for Parkinson's disease, and the treatments that do exist are limited in their ability to slow the disease's progress and alleviate the more advanced symptoms.
Scientists have "long recognized" that some nonmotor symptoms, such as those that affect the sense of smell and the gut, can appear before the motor stage of Parkinson's disease.
In addition, they have also established that the gut and brain are in constant communication with each other, mostly through the vagus nerve.
Braak's vagus nerve theory of Parkinson's
In 2003, the German brain researcher Heiko Braak proposed that the toxic journey of alpha-synuclein starts in the gut and spreads via the vagus nerve to the brain, where it wreaks havoc on dopamine cells.
Since then, a number of studies have found evidence to support Braak's theory, but until the most recent work, there had been no convincing animal models.
In the new study, Dawson and colleagues engineered a mouse model to demonstrate Braak's theory.
The muscles of the gut are rich in connections to the vagus nerve. So, the team injected preformed fibrils of alpha-synuclein into places in the gut muscles of the mice that were rich in vagus nerve connections.
The researchers note that the success of experiments depended not only on getting the site of injection just right but also on getting the right size and amount of fibrils.
"When the initial experiments started to work, we were utterly amazed," says Dawson, adding that "Now it is fairly routine for our research team."
TAG(s):
